Diethylene glycol
 | |
| Names | |
|---|---|
Preferred IUPAC name 2,2'-Oxydi(ethan-1-ol) | |
| Other names 2,2'-Oxybis(ethan-1-ol) 2-(2-Hydroxyethoxy)ethan-1-ol Diethylene glycol Ethylene diglycol Diglycol 2,2'-Oxybisethanol 2,2'-Oxydiethanol 3-Oxa-1,5-pentanediol Dihydroxy diethyl ether | |
| Identifiers | |
CAS Number |
|
3D model (JSmol) |
|
ChEBI |
|
ChemSpider |
|
ECHA InfoCard | 100.003.521 |
KEGG |
|
PubChem CID |
|
UNII |
|
InChI
| |
SMILES
| |
| Properties | |
Chemical formula | C4H10O3 |
Molar mass | 106.12 g/mol |
| Appearance | Colorless liquid |
Density | 1.118 g/mL |
Melting point | −10.45 °C (13.19 °F; 262.70 K) |
Boiling point | 244 to 245 °C (471 to 473 °F; 517 to 518 K) |
Solubility in water | miscible |
| Hazards | |
| Main hazards | Toxic |
Safety data sheet | Diethylene-glycol MSDS |
NFPA 704 |  1 1 0 |
| Related compounds | |
Related diols | ethylene glycol, triethylene glycol |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |
Infobox references | |
Diethylene glycol (DEG) is an organic compound with the formula (HOCH2CH2)2O. It is a colorless, practically odorless, poisonous, and hygroscopic liquid with a sweetish taste. It is miscible in water, alcohol, ether, acetone, and ethylene glycol.[1] DEG is a widely used solvent.[2] It can be a contaminant in consumer products; this has resulted in numerous epidemics of poisoning since the early 20th century.[1]
Contents
1 Preparation
2 Structure of DEG and related polyols
3 Uses
4 Toxicology
4.1 Toxicokinetics
4.1.1 Absorption and distribution
4.1.2 Metabolism and elimination
4.2 Mechanisms
4.3 Signs and symptoms
4.4 Treatment
4.5 Prognosis
5 Epidemiology
5.1 1937 – The Massengill Incident (United States)
5.2 1969 – South Africa
5.3 1985 – Spain
5.4 1985 – Wine scandal
5.5 1986 – India
5.6 1990 – Nigeria
5.7 1990–1992 – Bangladesh
5.8 1992 – Argentina
5.9 1995–1996 – Haiti
5.10 2006 – China
5.11 2006 – Panama
5.12 2007 – Worldwide toothpaste incident
5.13 2008 – Nigeria
6 See also
7 References
8 External links
Preparation
DEG is produced by the partial hydrolysis of ethylene oxide. Depending on the conditions, varying amounts of DEG and related glycols are produced. The resulting product is two ethylene glycol molecules joined by an ether bond.[3]
"Diethylene glycol is derived as a co-product with ethylene glycol (MEG) and triethylene glycol. The industry generally operates to maximize MEG production. Ethylene glycol is by far the largest volume of the glycol products in a variety of applications. Availability of DEG will depend on demand for derivatives of the primary product, ethylene glycol, rather than on DEG market requirements."[4]
Diethylene glycol is one of several glycols derived from ethylene oxide. Glycols related to and coproduced with diethylene glycol and have the formula HOCH2CH2(OCH2CH2)nOH are:
n = 0 ethylene glycol ("antifreeze"); monoethylene glycol MEG
n = 1 DEG
n = 2 triethylene glycol, TEG, or triglycol
n = 3 tetraethylene glycol
n = 4 pentaethylene glycol
n > 4 polyethylene glycol
These compounds are all hydrophilic, more so than most diols, by virtue of the ether functionality.
Uses
Diethylene glycol is used in the manufacture of saturated and unsaturated polyester resins, polyurethanes, and plasticizers.[5] DEG is used as a building block in organic synthesis, e.g. of morpholine and 1,4-dioxane. It is a solvent for nitrocellulose, resins, dyes, oils, and other organic compounds. It is a humectant for tobacco, cork, printing ink, and glue.[6] It is also a component in brake fluid, lubricants, wallpaper strippers, artificial fog and haze solutions, and heating/cooking fuel.[1] In personal care products (e.g. skin cream and lotions, deodorants), DEG is often replaced by selected diethylene glycol ethers. A dilute solution of diethylene glycol can also be used as a cryoprotectant; however, ethylene glycol is much more commonly used. Most ethylene glycol antifreeze contains a few percent diethylene glycol, present as an byproduct of ethylene glycol production.
Toxicology
Despite the discovery of DEG’s toxicity in 1937 and its involvement in mass poisonings around the world, the information available regarding human toxicity is limited. Some authors suggest the minimum toxic dose is estimated at 0.14 mg/kg of body weight and the lethal dose is between 1.0 and 1.63 g/kg of body weight,[7] while some suggest the LD50 in adults is of ~1 mL/kg,[1] and others suggest this is the LD30.[3] Because of its adverse effects on humans, diethylene glycol is not allowed for use in food and drugs. The U.S. Code of Federal Regulations allows no more than 0.2% of diethylene glycol in polyethylene glycol when the latter is used as a food additive.[8] The Australian government does not allow DEG as a food additive; it is only allowed at less than 0.25% w/w of DEG as an impurity of polyethylene glycol (PEG)[9] even in toothpaste.[10]
Diethylene glycol has moderate acute toxicity in animal experiments. The LD50 for small mammals has been tested at between 2 and 25 g/kg, less toxic than its relative ethylene glycol, but still capable of causing toxicity in humans. It appears diethylene glycol is more hazardous to humans than implied by oral toxicity data in laboratory animals.[1]
Toxicokinetics
Although there is limited information about toxicokinetics in humans, observations in mass poisonings and experimental studies suggest the following information:
Absorption and distribution
The principal method of absorption is through oral ingestion. Dermal absorption is very low, unless it is administered on broken or damaged skin. After ingestion, DEG is absorbed through the gastrointestinal tract and distributed by the bloodstream throughout the body, reaching peak blood concentrations within 30 to 120 minutes. Once DEG reaches the liver, it is metabolized by enzymes.[1][7]
Metabolism and elimination
At first, scientists thought that DEG metabolized into ethylene glycol, which is poisonous due to the metabolic production of glycolic acid, glyoxylic acid, and ultimately oxalic acid.[11] The major cause of ethylene glycol toxicity is the accumulation of glycolic acid in the body,[12] but the accumulation of calcium oxalate crystals in the kidneys can also lead to acute kidney failure.[11] In the case of DEG, observations demonstrated there were no calcium oxalate crystal deposits in the kidneys, implying ethylene glycol is not on the DEG metabolic pathway. Rat models suggest DEG is metabolized in the liver by enzyme NAD-dependent alcohol dehydrogenase (ADH) into a hydrogen ion, NADH and 2-hydroxyethoxyacetaldehyde (C4H8O3). Shortly after, 2-hydroxyethoxyacetaldehyde (C4H8O3) is metabolized by the enzyme aldehyde dehydrogenase (ALDH) into the weak acid 2-hydroxyethoxyacetic acid (HEAA) with chemical formula C4H8O4. Later on, HEAA leaves the liver through the bloodstream, being partially filtered in the kidneys for elimination.[1][7]
Mechanisms
Based on available literature, scientists suggest unmetabolized DEG and HEAA are partially reabsorbed through glomerular filtration. As a consequence, the concentrations of the weak acid HEAA and metabolites may cause renal delay, leading to metabolic acidosis and further liver and kidney damage.[1][7]
Signs and symptoms
The symptoms of poisoning typically occur in three characteristic intervals:[1]
First phase: Gastrointestinal symptoms, such as nausea, vomiting, abdominal pain, and diarrhea, develop. Some patients may develop early neurological symptoms like altered mental status, central nervous system depression, coma and mild hypotension.
Second phase: In one to three days after ingestion (and dependent on dose ingested), patients develop metabolic acidosis, which causes acute kidney failure, oliguria, increasing serum creatinine concentrations, and later anuria. Other symptoms reported and secondary to acidosis and/or renal failure are: hypertension, tachycardia, cardiac dysrhythmia, pancreatitis, hyperkalemia or mild hyponatremia.
Final phase: At least five to 10 days after ingestion, most of the symptoms are related to neurological complications, such as: progressive lethargy, facial paralysis, dysphonia, dilated and nonreactive pupils, quadriplegia, and coma leading to death.
Treatment
Fomepizole or ethanol should be quickly administered to prevent diethylene glycol being metabolized to the compound or compounds that cause the real damage.[1]
Fomepizole: an alcohol dehydrogenase (ADH) inhibitor with 8,000 times more affinity than ethanol. This treatment has minimal adverse effects because of constant serum concentration.[3] However, it is a very expensive medication (approximately $3,000 U.S. per treatment).[13]
Ethanol: ethanol is a competitive ADH substrate. A constant blood concentration of 1 to 1.5 g/L (corresponding to 0.5 to 0.75 mg/L in the breath) should be maintained to acceptably saturate the enzyme. An initial dose of 0.6 to 0.7 g ethanol per kilogram body weight should be given (ca 0.8 mL/kg or 0.013 fl.oz./lb). This will cause ethanol intoxication. To avoid adverse effects, frequent serum monitoring and dosage adjustments should be done.[1]
For late diagnosis where ethanol or fomepizole is ineffective, because DEG has already been metabolized, hemodialysis becomes the only treatment available.[3]
Hemodialysis might be administered alone or with ethanol or fomepizole.
Prognosis
The prognosis depends on prompt diagnosis and treatment due to the high mortality rate DEG intoxication produces. Patients who survive but develop renal failure remain dialysis-dependent. All patients are likely to suffer significant morbidity.[3]
Epidemiology
The physical properties of diethylene glycol make it an excellent counterfeit for pharmaceutical-grade glycerine (also called glycerol) or propylene glycol, and has caused many deaths in different countries. Incidents include its use in China as a component of cheap toothpaste, and by winemakers in Europe as an adulterant to create a "sweet" wine.[14][15]
1937 – The Massengill Incident (United States)
In 1937, S.E. Massengill Co. (a Tennessee drug company), manufactured sulfanilamide dissolved with diethylene glycol, to create a liquid alternative of this drug. The company tested the new product, Elixir Sulfanilamide, for viscosity, appearance and fragrance. At the time, the food and drug laws did not require toxicological analysis before releasing for sale. When 105 people died in 15 states during the months of September and October, the trail led back to the elixir, and the toxic potential of this chemical was revealed.[16][17][18] This episode was the impetus for the Federal Food, Drug, and Cosmetic Act of 1938.[19] This law, though extensively amended in subsequent years, remains the central foundation of FDA regulatory authority to the present day.[20]
1969 – South Africa
In Cape Town, South Africa, seven children developed vomiting, diarrhea, and dehydration, and died of renal failure after administration of over-the-counter sedatives. Soon, patients started to present anuria, acidic breathing, hepatomegaly, and unresponsiveness. Patients were treated with fluid hydration and correction of acidosis, but some were not able to survive. Postmortem examination revealed damage in the kidneys and liver, and laboratory testing found DEG instead of propylene glycol in the sedatives.[1][19]
1985 – Spain
Patients being treated for burns developed sudden anuric renal failure. Further investigation revealed all patients were treated with topical silver sulfadiazine ointment that contained 7 g/kg of DEG. This event caused the death of five patients.[3][21][22]
1985 – Wine scandal
During the month of July 1985, Austrian wines were found to contain up to 1,000 parts per million of DEG, giving them a desirable sweetness. Austrian wine was banned in many countries and the U.S. Bureau of Alcohol, Tobacco and Firearms started to test all imported wine.
In November, The New York Times published a wine recall that the Federal Government released after the Bureau of Alcohol, Tobacco and Firearms tested 1,000 bottles. 45 Austrian, 5 German and 12 Italian wines tested positive for DEG. Some wines contained less than 10 parts per million of DEG, a small amount that could not be detected by laboratory analysis in Europe. This triggered the installation of more sensitive laboratory equipment in Banafi laboratories, Italy, and stronger alcohol regulations in Austria.[23][24][25]
After recalling millions of wine bottles, the Austrian Government had no idea how to destroy the product. During September 1986, the Ministry of Public Works started testing a mixture of wine with salt to melt hazardous ice during winter. The primary results revealed that the mixture was more effective than using salt alone.[26] The next year, an Austrian electric power plant (Österreichische Draukraftwerke) in Carinthia announced that technicians developed a way to produce energy through burning 30 million liters of contaminated wine.[27]
1986 – India
At a hospital in Bombay, India, patients were admitted to be treated for diverse health problems. Doctors prescribed glycerine for its osmotic diuretic effect, but patients started to develop renal failure. Fourteen patients received hemodialysis, but the treatment failed. The episode resulted in the deaths of 21 patients and the discovery of glycerin contaminated with 18.5% v/v of DEG.[1][19][28]
1990 – Nigeria
During the summer months, 47 children were admitted to the Jos University teaching hospital, Nigeria, with anuria, fever and vomiting. The children later developed renal failure and died. All the children had received acetaminophen syrup to treat upper respiratory infections related with malaria. Once physicians identified a suspect paracetamol syrup, samples were shipped to the Centers for Disease Control and Prevention (CDC) in the U.S., which identified DEG. It was assumed that DEG was used as a substitute of propylene glycol, and this incident encouraged the Nigerian government to develop pharmaceutical quality control guidelines.[1][19][29][30]
1990–1992 – Bangladesh
In Bangladesh between 1990 and 1992, 339 children developed kidney failure, and most of them died, after being given paracetamol (acetaminophen) syrup contaminated with diethylene glycol. The outbreak forced the government to ban the sale of paracetamol elixirs in December 1992, causing a decline of 53% in the admission of patients with renal failure and an 84% decline in admissions by unexplained renal failure.[31]
1992 – Argentina
A propolis syrup manufactured by Huilen Laboratories in Buenos Aires, Argentina, contained between 24 and 66.5% DEG, and caused the death of 29 people.[32][33][34]
1995–1996 – Haiti
In the poorest country in the Western Hemisphere, diseases are not recognized unless they become large or unusual. Between November 1995 and June 1996, almost 109 children admitted to the University Hospital in Port-au-Prince, Haiti, presented with acute renal failure. By June 1996, with no idea what was causing the epidemic, the Pan American Health Organization (PAHO) Haiti representative contacted the World Health Organization (WHO, the parent agency of PAHO), and WHO requested that the Centers for Disease Control and Prevention investigate.[29][35][36]
Lead CDC investigator Dr. Katherine O'Brien conducted a case-control investigation, looking for potential clues to the epidemic. The study revealed a strong association between ingestion of two locally produced acetominophen liquid products (Afebril and Valodon) and illness. Laboratory testing at CDC of samples taken from parents revealed significant contamination with DEG.
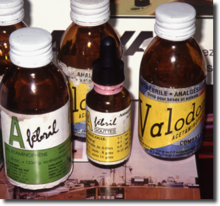
Medications contaminated with DEG
The factory of the medication manufacturer, Pharval, was subsequently investigated by Dr. Joel Selanikio (also of CDC, and an Epidemic Intelligence Service classmate of Katherine O'Brien). Testing of medication samples taken from the factory samples by both CDC and by an independent commercial lab located in Miami, revealed contamination by DEG of 16.4% and higher. With the available technology of the era, the CDC determined the glycerin used in the syrup preparation was contaminated with approximately 24% DEG.[29] As a result of the case-control findings, and subsequent investigation at the factory, public warnings were issues by the Ministry of Health and bottles of the two medications were taken from pharmacy shelves and destroyed. These measures quickly ended the advance of the epidemic.

Haiti 1996 DEG epidemic curve
Only 88 children deaths were recalled by doctors or had medical records. Nearly half of the victims were under the age of two.[37]
Ending June 1996, the FDA had discovered counterfeit glycerin traced back to Chemical Trading and Consulting (a German broker), which bought 72 barrels of the syrup from Vos B.V., a Dutch company. Vos records revealed the syrup had been bought from Sinochem International Chemicals Company through a German trader, Metall-Chemie. In July 1996, the American Embassy in China contacted Sinochem and requested a list of Chinese glycerin makers, but the company refused to reveal the names. It was not until September 1996 that Sinochem provided a name of the manufacturer of the tainted syrup. They identified Tianhong Fine Chemicals Factory as the manufacturer. While the FDA tried to find out Tianhong’s address, Chinese officials were reluctant to become involved. One year and a half after the FDA began to trace the poisonous shipments, an inspector, Ted Sze, finally visited the Tianhong Fine Chemicals Factory in Dalian, northeastern China. Once he was inside, there was nothing to do: the plant had already been shut down. The Dutch authorities assessed a $250,000 fine against Vos B.V., for not alerting anyone when they tested the syrup and found impurities.[37]
2006 – China
Wang Guiping discovered how easy it was to enter China’s pharmaceutical supply business and earn extra money. Records also revealed that to fool buyers, Wang falsified his license and laboratory analysis reports.
Wang declared that after making the first order of counterfeit syrup, he swallowed some of it. Once verifying that he was fine, he shipped it to Qiquihar No. 2 Pharmaceutical in 2005. Some time later, Wang found a reference to diethylene glycol in a chemical book. After manufacturing a second batch of syrup containing diethylene glycol for Qiquhar Pharmaceutical, no taste-test was performed. The counterfeit syrup ended in ampules of Amillarisin A, a medication for gall bladder problems; special pediatric enema fluid; blood vessel disease injections; intravenous pain reliever; and an arthritis medication.
In April 2006, the Guangdong Province Hospital of Guangzhou began administering Amillarisin A to their patients. Soon thereafter, patients died after receiving the medication. Mr. Wang was caught and Qiquihar was shut down by the authorities. Besides Wang, five employees of Qiquihar were prosecuted.[38]
2006 – Panama
Ending September 2006, the Arnulfo Arias Madrid Hospital at Panama City was getting full with patients with contradictory symptoms. The symptoms seemed to match with Guillain–Barré syndrome, but these patients were also losing their ability to urinate, a symptom not related to Guillain–Barré. The death rate of this mysterious illness was nearly 50%, when hospital management decided to isolate all the patients with the illness in a large room and doctors could compare notes and theories. Soon, patients from other parts of the country started to arrive at hospitals. Doctors had no idea what was happening: the mysterious illness was attacking elderly citizens with hypertension and diabetes history. About half were receiving Lisinopril (a blood pressure medicine), and many did not remember clearly if they had been taking other drugs. Suspecting something wrong with Lisinopril, the medicine was removed from the pharmacies[38] while the U.S. Food and Drug Administration conducted lab analyses, revealing the blood pressure drug was safe; CDC epidemiologists were then invited to participate.[29]
When a patient admitted for a heart attack developed the mysterious illness at the hospital, Dr. Nestor Sosa, an infectious disease specialist, analyzed the medical record. Because patients treated with Lisinopril developed a cough (a common side effect of ACE inhibitors), they were prescribed an expectorant.[38] Immediately, biological samples and the syrup were sent by jet to CDC for analysis. When urine analyses for a series of metals, pesticides or their metabolites resulted negative, CDC scientists recalled the Nigeria and Haiti incidents. The CDC employed modern laboratory equipment to analyze the samples and confirm the results: the samples contained approximately 8% v/v DEG. Later, raw glycerin was analyzed and results revealed 22.2% v/v DEG.[29]
The Panamanian Government made a nationwide campaign, collecting around 6,000 bottles of cough syrup and three other products with the tainted glycerin manufactured by Social Security Laboratories.[39] The 46 barrels of syrup were bought by Social Security Laboratories through a Panamanian middleman, Grupo Comercial Medicom, who bought the product from Rasfer Internacional, a Spanish company. In fact, Rasfer received the product from CNSC Fortune Way, which in turn bought it from the Taixing Glycerine Factory. At the request of the United States, the State Food and Drug Administration of China investigated Taixing Glycerine Factory and CNSC Fortune Way, but the agency concluded it is not under their jurisdiction because the factory is not certified to make medicine.[38][40]
Taixing sold the syrup as “TD glycerin”, wording that neither Chinese inspectors nor Spanish medical authorities comprehended. Unfortunately, Taixing used “TD” for the Chinese word tidai, meaning “substitute”.[38] A New York Times reporter tried to obtain a comment from CNSC Fortune Way at the CPhI worldwide (the world’s largest annual pharmaceutical convention) held in Milan, Italy, during 2007, but their representatives refused to comment.[41]
In August 2009, the Supreme Court decided to send the diethylene glycol file to the Public Ministry for an extension.[42] The following month, the Toxicology Department of the Institute of Legal Medicine and Forensic Science published a list of 1,155 names whose medicine bottles tested positive for DEG. Only approximately 3,000 bottles had been analyzed from the total 6,000 bottles collected. The fiscal attorney urged affected citizens to approach the Public Ministry to update the official legal file and for further medical analysis.[39] Two months later, findings revealed that 145 were proven to die by DEG intoxication, but the DA still has to investigate 953 demands.[43]
The New York Times reported that Taixing was closed by the Chinese government and CNSC Fortune Way, which is also owned by the Chinese government, was never sanctioned.[41] In Spain, Rasfer International declared bankruptcy after the lawyer of Medicom filed a lawsuit of $400 million in July 2008.[44] Spanish authorities are prosecuting Asunción Criado, general manager of Rasfer Internacional, S.A., and await Panamanian citizens, René Luciani (former Social Security Director) and Jéssica Rodríguez (former Purchase National Director) for their hearings. Meanwhile, in Panama, De la Cruz, legal representative of Medicom, remains in jail pending a trial. Seventeen other persons have also been charged related to this incident. Panama awaits the extradition of Criado for her hearing.[45]
Panama’s case made CDC set standardized methodology for DEG identification, hoping to have more timely response in future events. The agency also identified urinary DEG as a biomarker for DEG exposures.[29] The United States Food and Drug Administration also issued an Industry Guidance Document “intended to alert pharmaceutical manufacturers, pharmacy compounders, repackers, and suppliers to the potential public health hazard of glycerin contaminated with diethylene glycol (DEG)” and recommended appropriate testing procedures for the use of glycerin.[46]
During June 2011, the number of confirmed deaths according to the official list rose to 219 victims [47]
2007 – Worldwide toothpaste incident
In May 2007, a Panamanian named Eduardo Arias discovered a 59-cent toothpaste that was labeled containing DEG. Panamanian officials traced the toothpaste to a local company in the Colón Free Trade Zone. In fact, the company bought the product in China and had already re-exported toothpaste to Costa Rica, Dominican Republic and Haiti, making Panama kick off a local warning.[48][49][50] For the end of the month, the Chinese government committed to investigate the “supposedly” tainted toothpaste that had been recalled in Panama and Dominican Republic, but stated that, as per an essay written in 2000, a toothpaste containing 15.6% was not dangerous.[51]
On June 1, 2007, the FDA warned consumers to avoid toothpaste from China, although there was no information if these toothpastes had already entered the US, and started testing any imported Chinese toothpaste.[52][53] Days later, Colgate-Palmolive found counterfeit toothpaste with its name, which was contaminated with DEG and found at dollar-type discount stores in New York, New Jersey, Pennsylvania and Maryland. The toothpaste was labeled as “Manufactured in South Africa” and contained misspellings like "isclinically", "SOUTH AFRLCA" and "South African Dental Assoxiation".[54][55] Although there were no reports of anyone harmed, several people in the eastern US reported experiencing headaches and pain after using the product.[56] It was later discovered that a great number of tubes with poison ended up in hospitals for the mentally ill, prisons, juvenile detention centers, other hospitals and many other state institutions.[57]
In July 2007, England detected a counterfeit Sensodyne toothpaste on sale at a car boot sale in Derbyshire.[58] Soon, authorities in Belize, Canada, Mozambique, Saudi Arabia, New Zealand, Spain, Italy, Japan, Ireland and an Indianapolis, Indiana US hotel supplier that distributed Chinese toothpaste in Barbados, Belgium, Bermuda, Britain, Canada, Dominican Republic, France, Germany, Ireland, Italy, Mexico, Spain, Switzerland, Turks and Caicos, the United Arab Emirates and United States were also recalling Chinese-made toothpaste. What began as a local alert revealed a global problem in more than 30 countries and involving more than thirty brands.[59] The world outcry made Chinese officials ban the practice of using diethylene glycol in toothpaste.[60]
2008 – Nigeria
Ending November 2008, infants started to die after developing unexplained fevers and vomiting. Investigations revealed that all had taken a medicine called “My Pikin Baby”, a teething mixture tainted with diethylene glycol. The poison had caused the death of at least 84 Nigerian children between ages of two months and seven years.[61][62]
The Nigerian government traced the diethylene glycol to an unlicensed chemical dealer in Lagos, who sold it to a local pharmaceutical manufacturer. Barewa Pharmaceuticals was shut down and the product was pulled off the shelves. They also arrested 12 people in connection with the incident. This being the second incident involving counterfeit glycerine, it prompted the Nigerian National Agency for Food And Drug Administration and Control (NAFDAC) to adopt zero tolerance for counterfeits.[63][64][65]
See also
- Counterfeit medications
- Ethylene
- Ethylene glycol poisoning
- Polyethylene glycol
References
^ abcdefghijklmn Schep LJ, Slaughter RJ, Temple WA, Beasley DM (2009). "Diethylene glycol poisoning". Clin Toxicol. 47 (6): 525–35. doi:10.1080/15563650903086444. PMID 19586352..mw-parser-output cite.citation{font-style:inherit}.mw-parser-output q{quotes:"""""""'""'"}.mw-parser-output code.cs1-code{color:inherit;background:inherit;border:inherit;padding:inherit}.mw-parser-output .cs1-lock-free a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/6/65/Lock-green.svg/9px-Lock-green.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-lock-limited a,.mw-parser-output .cs1-lock-registration a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/d/d6/Lock-gray-alt-2.svg/9px-Lock-gray-alt-2.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-lock-subscription a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/a/aa/Lock-red-alt-2.svg/9px-Lock-red-alt-2.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration{color:#555}.mw-parser-output .cs1-subscription span,.mw-parser-output .cs1-registration span{border-bottom:1px dotted;cursor:help}.mw-parser-output .cs1-hidden-error{display:none;font-size:100%}.mw-parser-output .cs1-visible-error{font-size:100%}.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration,.mw-parser-output .cs1-format{font-size:95%}.mw-parser-output .cs1-kern-left,.mw-parser-output .cs1-kern-wl-left{padding-left:0.2em}.mw-parser-output .cs1-kern-right,.mw-parser-output .cs1-kern-wl-right{padding-right:0.2em}
^ Siegfried Rebsdat and Dieter Mayer "Ethylene Glycol" in Ullmann’s Encyclopedia of Industrial Chemistry, 2002, Wiley-VCH, Weinheim.doi:10.1002/14356007.a10_101.
^ abcdef Marraffa JM, Holland MG, Stork CM, Hoy CD, Hodgman MJ (2008). "Dietylene Glycol: Widely Used Solvent Presents Serious Poisoning Potential". J Emerg Med. 35 (4): 401–406. doi:10.1016/j.jemermed.2007.06.025. PMID 18024066.
^ http://www.chemicalland21.com/petrochemical/DEG.htm
^ Diethylene Glycol
^ O’Neil M. The Merck Index. 14th ed. Whitehouse Station, NJ: Merck & Co; 2006.
^ abcd Kraut JA, Kurtz I (2008). "Toxic alcohol ingestions: clinical features, diagnosis, and management". Clin J Am Soc Nephrol. 3 (1): 208–225. doi:10.2215/CJN.03220807. PMID 18045860.
^ ADDITIVES PERMITTED FOR DIRECT ADDITION TO FOOD FOR HUMAN: Polyethylene glycol, Code of Federal Regulations, Title 21, Vol.3, Part 172, Sec. 172.820, Revised as of April 1, 2006
^ Existing Chemical Hazard Assessment Report, June 2009
^ Australian Competition and Consumer Commission. "Toothpaste containing more than 0.25 per cent by weight of diethylene glycol (DEG)". Archived from the original on 21 June 2009. Retrieved 1 December 2009.
^ ab Brent, J. (2001). "Current Management of Ethylene Glycol Poisoning". Drugs. 61 (7): 979–88. doi:10.2165/00003495-200161070-00006. ISSN 0012-6667. PMID 11434452.
^ Clay, K. L.; Murphy, R. C. (1977). "On the Metabolic Acidosis of Ethylene Glycol Intoxication". Tox. Appl. Pharm. 39 (1): 39–49. doi:10.1016/0041-008X(77)90175-2. ISSN 0041-008X. PMID 14421.
^ Internal Medicine Residency Program of the College of Medicine of Wake Forest University, North Caroline, U.S.A. Retrieved December 8, 2009.
^ van der Linden-Cremers PM, Sangster B (1985). "Medical sequelae of the contamination of wine with diethylene glycol". Ned Tijdschr Geneeskd (in Dutch). 129 (39): 1890–1. PMID 4069248.
^ Authorities warn against using some toothpastes, GulfNews, Published 04/06/2007
^ Ballentine, C. Taste of Raspberries, Taste of Death – The 1937 Elixir Sulfanilamide Incident. FDA Consumer Magazine, June 1981.
^ "Medicine: Post-Mortem". Time magazine. December 20, 1937. Retrieved 2009-07-19.Then, two months ago, fatality knocked at its door. A new mixture of a new drug (sulfanilamide) with a new solvent (diethylene glycol), which Dr. Massengill's salesmen sold as Elixir Sulfanilamide-Massengill, was discovered to be killing its users
^ "Wallace Reveals How Federal Agents Traced Elixir to Halt Fatalities". The New York Times. November 26, 1937. Retrieved 2009-07-20.A graphic story of a race against death from "elixir sulfanilamide," carried on by the Food and Drug Administration in fifteen States from Virginia to California, a race not won until ninety-three persons had died after taking the lethal dose, was told by Secretary Wallace today in a report responding to Senate and House resolutions.
^ abcd Wax PM. (1995). "Elixirs, diluents, and the passage of the 1938 Federal Food, Drug and Cosmetic Act". Ann Intern Med. 122 (6): 456–61. doi:10.7326/0003-4819-122-6-199503150-00009. PMID 7856995.
^ The History of FDA at FDA.gov
^ Schier JG, Rubin CS, Miller D, Barr D, McGeehin MA (2009). "Medication-associated diethylene glycol mass poisoning: A review and discussion on the origin of contamination". J Public Health Policy. 30 (2): 127–143. doi:10.1057/jphp.2009.2. PMID 19597445.
^ Cantarell MC, Fort J, Camps J, Sans M, Piera L (Mar 1987). "Acute intoxication due to topical application of diethylene glycol". Ann Intern Med. 106 (3): 478–9. doi:10.7326/0003-4819-106-3-478_2. PMID 3813252.
^ Molotsky, I. "Popular Wines found to hold toxic chemical." The New York Times. November 1, 1985. Retrieved December 8, 2009.
^ Tagliabue, J. "Scandal over poisoned wine embitters village in Austria." The New York Times. August 2, 1985. Retrieved December 8, 2009.
^ Bureau of Alcohol, Tobacco, and Firearms. Industry Circular No. 86-13. October 6, 1986. Retrieved December 8, 2009.
^ "Tainted wine clear roads." Wilmington Morning Star. December 22, 1986. Retrieved December 9, 2009.
^ Reuter. "Austrian power plant to burn 'bad' wine." February 27, 1987. Retrieved December 9, 2009
^ Pandya SK (1988). "Letter from Bombay. An unmitigated tragedy". BMJ. 297 (6641): 117–9. doi:10.1136/bmj.297.6641.117. PMC 1833772. PMID 3408933.
^ abcdef Barr DB, Barr JR, Weerasekera G, Wamsley J, Kalb SR, Sjödin A, Schier JG, Rentz ED, Lewis L, Rubin C, Needham LL, Jones RL, Sampson EJ (2007). "Identification and quantification of diethylene glycol in pharmaceuticals implicated in poisoning epidemics: an historical laboratory perspective". J Anal Toxicol. 31 (6): 295–303. doi:10.1093/jat/31.6.295. PMID 17725874.
^ Okuonghae HO, Ighogboja IS, Lawson JO, Nwana EJ (1992). "Diethylene glycol poisoning in Nigerian children". Ann Trop Paediatr. 12 (3): 235–8. PMID 1280035.
^ Hanif M, Mobarak MR, Ronan A, Rahman D, Donovan JJ Jr, Bennish ML (1995). "Fatal renal failure caused by diethylene glycol in paracetamol elixir: the Bangladesh epidemic". BMJ. 311 (6997): 88–91. doi:10.1136/bmj.311.6997.88. PMC 2550149. PMID 7613408.
^ Ferrari LA, Giannuzzi L (2005). "Clinical parameters, postmortem analysis and estimation of lethal dose in victims of a massive intoxication with diethylene glycol". Forensic Sci Int. 153 (1): 49–51. doi:10.1016/j.forsciint.2005.04.038. PMID 15979833.
^ Schep LJ, Slaughter RJ (2005). "Comments on diethylene glycol concentrations". Forensic Sci Int. 155 (2–3): 233. doi:10.1016/j.forsciint.2005.08.001. PMID 16171962.
^ "Toll reaches 20 in tonic poisoning." Akron Beacon Journal (OH). August 22, 1992. Retrieved December 8, 2009.
^ O'Brien KL, Selanikio JD, Hecdivert C, Placide MF, Louis M, Barr DB, Barr JR, Hospedales CJ, Lewis MJ, Schwartz B, Philen RM, St Victor S, Espindola J, Needham LL, Denerville K. (1998). "Epidemic of pediatric deaths from acute renal failure caused by diethylene glycol poisoning". JAMA. 279 (15): 1175–80. doi:10.1001/jama.279.15.1175. PMID 9555756.CS1 maint: Multiple names: authors list (link)
^ "Fatalities Associated with Ingestion of Diethylene Glycol-Contaminated Glycerin Used to Manufacture Acetaminophen Syrup — Haiti, November 1995 – June 1996" (PDF). Morbidity and Mortality Weekly Report. 1996.
^ ab Bogdanich, W. (June 2007). "FDA Tracked Poisoned Drugs, but Trail went cold in China". The New York Times.
^ abcde Bogdanich, W; Hooker, J. (June 2007). "From China to Panama, a trail of Poisoned Medicine". The New York Times.
^ ab Otero, J. (Sep 2009). "Aumentan Envenenados con Dietilene Glycol".
^ Rentz ED, Lewis L, Mujica OJ, Barr DB, Schier JG, Weerasekera G, Kuklenyik P, McGeehin M, Osterloh J, Wamsley J, Lum W, Alleyne C, Sosa N, Motta J, Rubin C. (2008). "Outbreak of acute renal failure in Panama in 2006: a case-control study" (Free full text). Bull World Health Organ. 86 (10): 749–56. doi:10.2471/BLT.07.049965. PMC 2649516. PMID 18949211.CS1 maint: Multiple names: authors list (link)
^ ab Harris, R. (October 2007). China's Unwatched Drug Makers. The New York Times.
^ Otero, J. (Aug 2009). "Caso dietilene glycol puede viciarse: Troitiño".
^ Otero, J. (November 2009). "24 Niños afectados por utilización de tóxico".
^ Perez, R. (July 2008). "Rasfer Internacional se declara en bancarrota". Archived from the original on 2011-09-28.
^ Irujo, J. (Jul 2009). "Panamá bloquea el proceso español por el caso del jarabe asesino".
^ Guidance for Industry – Testing of Glycerin for Diethylene Glycol
^ http://mensual.prensa.com/mensual/contenido/2011/06/28/hoy/panorama/2646054.asp
^ Bogdanich, W.; McLean, R. "Poisoned Toothpaste in Panama Is Believed to Be From China", The New York Times, May 19, 2007.
^ "China investigating toothpaste containing potentially deadly chemical". International Herald Tribune. 2007-05-22. Retrieved 2007-05-22.
^ "U.S. checking all toothpaste imports from China". CNN. 2007-05-23. Archived from the original on 2007-05-26. Retrieved 2007-05-23.
^ Xiaomin, X; Hongyi, W. (2007-05-24). "Gov't probes 'tainted toothpaste' case". China Daily. Retrieved 2009-12-10.
^ Bogdanich, W. "Toxic Toothpaste Made in China Is Found in U.S. ", The New York Times, June 2, 2007.
^ U.S. Food and Drug Administration Press Release. "FDA Advises Consumers to Avoid Toothpaste From China Containing Harmful Chemical. FDA Detains One Contaminated Shipment, Issues Import Alert", June 1, 2007.
^ Colgate Palmolive Company Press Release. "Counterfeit Colgate Toothpaste Found", June 14, 2007.
^ U.S. Food and Drug Administration Press Release. "Counterfeit Colgate Toothpaste Found", June 14, 2007.
^ 7online.com: Toothpaste recall expands 6/18/07
^ Bogdanich, W. "Wider Sale Is Seen for Toothpaste Tainted in China ", The New York Times, June 28, 2007.
^ "Toxin found in fake UK toothpaste". BBC News. July 12, 2007. Retrieved May 1, 2010.
^ "Tainted toothpaste across the world", The New York Times, September 30, 2007.
^ Bogdanich, W. "The Everyman Who Exposed Tainted Toothpaste", The New York Times, October 1, 2007.
^ News.yahoo.com Nigeria child deaths from tainted syrup rise to 84
^ Nigeria child deaths from tainted syrup rise to 84
^ "Nigeria: 12 Held Over Tainted Syrup". The New York Times. February 12, 2009. Retrieved May 1, 2010.
^ Polgreen, Lydia (February 7, 2009). "84 Children Are Killed by Medicine in Nigeria". The New York Times. Retrieved May 1, 2010.
^ NAFDAC Negotiates State of the art Anti Counterfeiting Equipment
- Sources
Merck Index, 12th Edition, 3168.
External links
- The Elixir Sulfanilamide Disaster